“Whoever said nothing is impossible obviously hasn't tried nailing Jell-O to a tree.”—John Candy
As the year comes to a close, there are many lists of the best and worst in almost every imaginable category for 2014. Here at Health AGEnda, we have made an annual practice of reviewing the workforce in training data—specifically, the number of graduating resident physicians choosing additional training in geriatric fellowship programs—published in the Journal of the American Medical Association (JAMA). (Read Boxing Day Brings Glad Tidings for Geriatrics Field from 2013, Decline in Geriatric Fellows Defies Pay Boost: +10% = -10% from 2012 and Falling Leaves, Falling Numbers from 2011.)
I recently saw one of my charts presented (without attribution :-( ) in a Washington briefing session on the workforce available to care for older adults, so I guess I have to keep updating them.
I find the data on physicians in training useful as a way of reflecting on the progress of geriatric medicine—and, by extension, geriatric specialization in all of the health professions. Unfortunately, I’m quite confident that rates of geriatric specialization in any field are responding to the same interrelated forces: perceived status, pay, perceived utility of the specialized knowledge, and awareness of the option. There is just better data in medicine, although it is still somewhat lagged, reflecting academic 2013-14 rather than the current 2014-15.
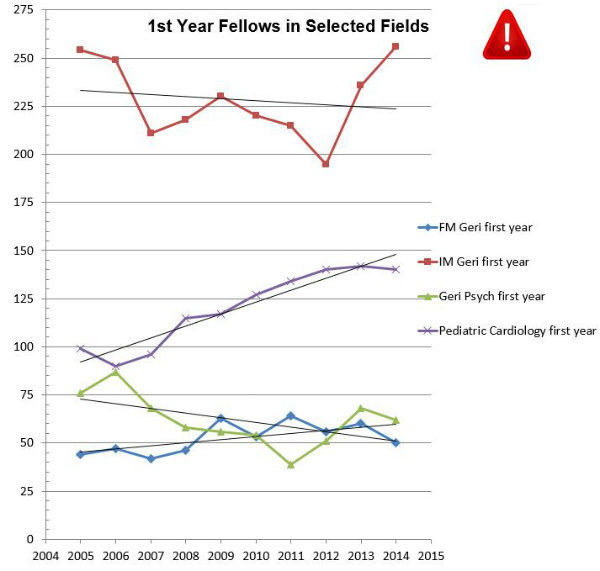 Chart by Chris Langston
Chart by Chris LangstonAs in recent years, the news is very mixed. If you look at the accompanying chart, the number of first-year fellows in geriatric Internal Medicine is up by 20, from 236 to 256 (an increase of almost 9 percent), returning the field to where it stood in 2005 (plus two people). Unfortunately, the number of first-year fellows training in Family Medicine-sponsored programs fell by 10—an alarming decrease (from 60 to 50) in this smaller branch of the field. Geriatric Psychiatry also gave up some ground, falling from 68 back to 62 but still well above its 2011 nadir of 39. For context, I have been graphing the growth of the field of Pediatric Cardiology—which seems to have leveled off, finally, in 2014.
As a share of all physicians in graduate training, each of these geriatric disciplines represents between .1 percent and .2 percent of total residents in training (.001 - .002), which is the modal number for most advanced fellowship programs. Among internal medicine specialties, geriatric medicine is actually more popular than rheumatology (205 first-year fellows) but below the next smallest: infectious disease (272) and nephrology (437). Compared to sports medicine, the other certificate of added qualification in Family Medicine, geriatrics is one-third the size: 50 versus 166. In psychiatry, geriatrics is on a par with addiction (59), forensic (63), and psychosomatic (75) specialties, but dwarfed by child and adolescent (390).
However, missing from all of this description of what is is the ought. What should the numbers be? Right now, we are not even training enough physicians in geriatrics to keep the numbers of those with certification steady at around 7,000—although this is something of an artifact of the bulge in physicians certifying in geriatrics in advance of the formal fellowship requirement, many of whom are not recertifying in the field, but not necessarily leaving practice.
I recently made up a rule of thumb derived from the work of the American Geriatrics Society (AGS) suggesting that there should be one geriatrician for every 2,200 persons 65 and older (arguing that 30 percent of people 65 and up have complex enough needs to warrant specialized care, and the proper panel size for this care would be 700). If there are approximately 44.5 million people over 65, that ratio would yield a target number of 20,000 geriatricians. Others have reached similar conclusions with different population segmentation and panel size assumptions.
To achieve this target would require training more than 2,500 geriatricians per year for 10 years, to not only maintain but expand the workforce, followed by a reduction to replacement rate.
Given that this would be almost 10 times our current production of geriatricians and that there do not seem to be any practical approaches to changing output to this level, we may as well try nailing Jell-O to a tree.
I think we have to conclude that we need to change the game if we are to have any hope of winning. We need to make our numerical disadvantage irrelevant to our desired outcomes.
In the John A. Hartford Foundation’s new strategic plan, we have therefore shifted from an emphasis on the numbers of health care professionals with expertise in geriatric care to an effort to arm those we do have with additional skills to be effective. Their jobs will be to make excellent geriatric care the default process of care delivered by non-specialists.
Given the numbers, we need each geriatrics expert to have an impact equivalent of four people. We believe that by focusing on using their expertise to design clinical systems, manage practice change, and participate in the policy process, we can leverage their precious skills and still succeed in improving the health of older Americans.
