Normally one of the advantages of expecting the worst is that all one’s surprises are good ones. But this year, I am both surprised and dismayed at the new figures on physician enrollment in geriatric fellowship training reported in the December 5 education issue of the Journal of the American Medical Association.
Somehow, despite all of the hullabaloo surrounding health reform, which has done some very good things for pay and attention given to geriatrics and geriatricians, the number of first-year fellows has fallen again from last year’s precarious situation, discussed in Falling Leaves, Falling Numbers.
While the number of internal medicine-based fellowship programs has risen by one (from 104 to 105), the number of first-year fellows has fallen from last year’s reported 215 down to 195, a drop of nearly 10 percent. Similarly, the number of family medicine-based programs has increased by one and the number of first-year fellows has fallen from 64 to 56.
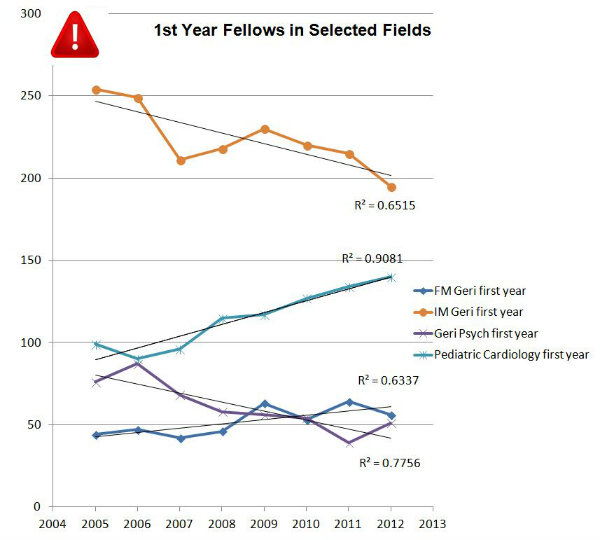
Just a note: The numbers basically lag one year behind the report. So the numbers reported this month reflect fellowship enrollments as of December 2011. So whereas in December 2010, there were 279 fellows in their first year of geriatrics training, in December 2011, there were 251!
What makes this all the more shocking is that—as announced late in 2010 and implemented in 2011—generalist physicians (including geriatricians) caring for Medicare beneficiaries and billing on outpatient evaluation and management codes got a 10 percent bonus on their reimbursement for their services. The American College of Physicians estimates that for its general internal medicine members, the bonus might amount to an increase in revenue of as much as $8,000 in a year. Since the usual numbers we cite say that older adults represent ~30 percent of the visits to a general internist, this would imply that a geriatrician should take in three times that much additional revenue, or $24,000 for the year.
Given that these bonuses require no new services or work and, as far as I can tell, little or no additional documentation, geriatricians should have seen an increase in net revenue from billings equivalent to more than 10 percent of the salary compensation of the average geriatrician. And yet the number of people electing to join the roles of geriatricians actually fell. This is not how I had heard supply and demand was supposed to work.
Obviously, there is a lot of noise and lag in the system regarding payments. I am sure that screams and hollers about the repeatedly impending imposition of the sustainable growth rate cut on part B physician payments under Medicare were a lot louder than the cries of gratitude for the pay increases. In fact, a quick search of the American Geriatrics Society/Association of Directors of Geriatric Academic Programs websites show no information about what geriatricians might stand to gain from the bonus program. And certainly not the wall-sized printable giant poster I had imagined showing some famous geriatrician pointing at the viewer and saying “I want you … to become a geriatrician and earn more money!”
Timing also counts. People in first-year geriatric fellowships in December will have made their choices somewhere in the preceding 18 months for all but the most competitive programs and may have made their career trajectory decisions much earlier. That means even fellows in training as of December 2011 may not have had enough advance notice about increasing pay to respond by favoring fellowships in geriatrics. So maybe next year, things will be better. Maybe.
There is some good news. Already things are better for geriatric psychiatry. Whereas the 55 programs in geriatric psychiatry had 39 fellows in first-year training in the 2011 report, this year there were 51. A 20 percent increase! I don’t know what they had for breakfast, but I want some, too. Congratulations to geriatric psychiatry program directors! Now, do it again!
Oh, and by the way, pediatric cardiology, which we used as a comparison case in last year’s discussion of these issues, increased its first-year fellows by almost 5 percent, from 134 to 140.
