 Let’s say you are 80 years old and about to undergo surgery. Perhaps it was an unexpected fall that placed you in the emergency department and you’ll need an orthopedic surgeon to repair your hip. You’ll undergo anesthesia during the procedure and afterwards will likely require rehab.
Let’s say you are 80 years old and about to undergo surgery. Perhaps it was an unexpected fall that placed you in the emergency department and you’ll need an orthopedic surgeon to repair your hip. You’ll undergo anesthesia during the procedure and afterwards will likely require rehab.
All of the physicians who might care for you—from the ER doc to the anesthesiologist to the physical medicine/rehab physician—have spent years and years of training to specialize in their discipline.
But do they know about the drugs that should be avoided in older patients? Do they appropriately assess for frailty or cognitive impairment? Do they understand the risk factors for post-operative delirium (an acute state of confusion) and how to mitigate them?
Unfortunately, too many surgical and related specialists haven’t received adequate training in how best to care for older patients, who—like the pediatric population—have different needs than the general adult patient.
Fortunately, there are tools to help specialists do better.
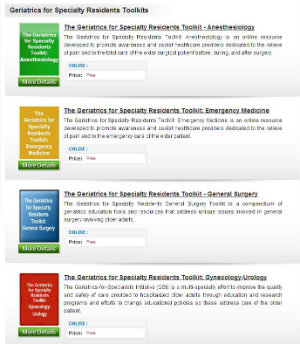 Click image to visit the Geriatrics for Specialty Residents Toolkits site.
Click image to visit the Geriatrics for Specialty Residents Toolkits site.The American Geriatrics Society has posted eight free toolkits of geriatrics educational materials that can be used in residency training for surgeons and other related specialists. Curriculum and rotation manuals, slide sets, lecture notes, learner assessments, and other resources are available for resident training programs in anesthesiology, emergency medicine, general surgery, gynecology-urology, ophthalmology, orthopedic surgery, otolaryngology, and physical medicine/rehabilitation.
These toolkits were made possible through the Geriatrics for Specialists Initiative (GSI), which for 20 years has been working to improve care delivered to older adults by surgical and related specialists. A component of the program funded 90 specialty residency programs across the country to work on improving their curriculum so that physicians in the early years of their supervised practice get the skills they need to care for older adults.
The fruits of their labor have now been collected into these searchable toolkits that can be shared easily online via the American Geriatrics Society and POGOe, a geriatrics education site.
For practicing surgical specialists and hospitals, another valuable resource is the Best Practice Guidelines for Optimal Preoperative Assessment of the Geriatric Surgical Patient, developed through the GSI in partnership with the American College of Surgeons. With the numbers of elderly surgery patients growing dramatically, this kind of guidance can help hospitals ensure they are delivering the best possible care to older adults.
Stay tuned for a peri-operative best practices guideline and a delirium-specific guideline now in development. And for emergency medicine, new geriatric emergency department guidelines can provide a way of embedding good geriatric care in an emergency room.
We really need a new paradigm for care of high-risk surgical patients who are often older adults with complex health conditions.
For our readers working in hospitals and academic medical centers around the country, we hope you will reach out and share these resources with your specialty colleagues and clinician-educators who have responsibility for training future orthopedic surgeons, anesthesiologists, and other specialists.
And if you are one of our many Hartford-supported, geriatrics-expert health care professionals, we hope you will be welcomed with open arms for the important knowledge you bring about older adults who might end up on the operating table.
As a recent New England Journal of Medicine piece argues, we really need a new paradigm for care of high-risk surgical patients who are often older adults with complex health conditions. We need to do better in educating patients and providers about the risks and benefits of surgery and helping people make the right decisions about whether to have procedures.
For those complex older adults who do choose surgery, interdisciplinary and geriatrically expert teams must work together to produce the best possible outcomes. If I was an 80-year-old undergoing hip fracture surgery, I’d want nothing less.
This is the ninth in an occasional series. See other Health AGEnda posts on Tools You Can Use:
Tools You Can Use: Geriatric Transitions Objective Structured Video Examination
Tools You Can Use: A New APProach to Treating Older Patients
Tools You Can Use: Detecting Cognitive Impairment During the Medicare Annual Wellness Visit
Tools You Can Use: Preparing a Personal Advance Care Plan
Tools You Can Use: Guidelines for Assessing Patients Facing Surgery
Tools You Can Use: Principles for Treating Patients with Multiple Chronic Conditions
