On June 1, the Foundation had the privilege of co-sponsoring (along with The Atlantic Philanthropies and The Robert Wood Johnson Foundation) a convening organized by Community Catalyst to discuss the ambitious new plans afoot to radically redesign how care is delivered and financed for the "duals"--those low income and largely frail people who are eligible for both Medicare and Medicaid.
On June 1, the Foundation had the privilege of co-sponsoring (along with The Atlantic Philanthropies and The Robert Wood Johnson Foundation) a convening organized by Community Catalyst to discuss the ambitious new plans afoot to radically redesign how care is delivered and financed for the "duals"--those low income and largely frail people who are eligible for both Medicare and Medicaid.
 These plans are the fruits of initiatives sponsored by the new Federal Medicare-Medicaid Coordination Office (known as the Office of the Duals) and are intended to integrate primary, acute, and long-term care and their federal and state payment streams. In some ways this initiative is one of the boldest in all of health reform, with the potential to improve care for millions of the neediest (and most expensive) people and reduce some of the billions of dollars currently spent on fragmented and uncoordinated care. For many in the field of aging and health this integration is "The Holy Grail" — heretofore only glimpsed in relatively small scale at PACE sites (the Program of All-inclusive Care for Elders) and a few other oddities. Of course I am in favor of finding the Holy Grail…if we choose the right cup. Yet we are on the verge of putting millions of people into new but untested financing and delivery models in a period of unprecedented budget strain and near financial desperation.
These plans are the fruits of initiatives sponsored by the new Federal Medicare-Medicaid Coordination Office (known as the Office of the Duals) and are intended to integrate primary, acute, and long-term care and their federal and state payment streams. In some ways this initiative is one of the boldest in all of health reform, with the potential to improve care for millions of the neediest (and most expensive) people and reduce some of the billions of dollars currently spent on fragmented and uncoordinated care. For many in the field of aging and health this integration is "The Holy Grail" — heretofore only glimpsed in relatively small scale at PACE sites (the Program of All-inclusive Care for Elders) and a few other oddities. Of course I am in favor of finding the Holy Grail…if we choose the right cup. Yet we are on the verge of putting millions of people into new but untested financing and delivery models in a period of unprecedented budget strain and near financial desperation.
Ready, Fire…Aim?
I've reviewed 3 of the 26 state plans--Ohio, California, and New York--and I have some real concerns. Clearly the states are much more familiar with the Medicaid only and Medicaid-disabled populations than they are with the majority, the older adult dual eligible beneficiaries. There is very little attention to end-of-life issues, palliative care needs, or even regular nursing homes in the plans. They have high hopes for electronic health records and information sharing among providers that I don't think are realistic within 6 months. There are blithe references to health or medical "homes" — the actual evidence for which is sparse to negative in the older adult population.
Nevertheless, the plans are very ambitious: Ohio wants to enroll in its "demonstration" some 114,000 of its 180,000 duals; California wants to enroll 685,000 of 1,100,000 duals in an eight-county region; and New York wants to enroll 250,000 of 755,000 duals. Ohio and California want to implement their plans by January 2013, while New York wants half by 2013 and the other half by 2014. I'm not sure we can realistically call these "demonstrations," especially as the states' plans already call for further expansion without any time to breath, evaluate, and revise the current approaches based on their results.
Finally, I am most concerned by the fact that quality measurement plans for these new managed care plans are sparse (Ohio and New York) to non-existent (California). In capitated insurance plans where the payor (i.e., the state and the federal governments) prepays an entity to take full risk for costs of care and full responsibility for the quality and adequacy for care, how one measures quality is essential. Otherwise the incentives to deny care can be overwhelming. And in this special population, I think the usual rehashing of HEDIS (Healthcare Effectiveness Data and Information Set) disease-focused measures such as Hemoglobin A1c control in diabetics or colonoscopy screening rates just doesn't cover the information we need. Ohio's proposed measures look the best of the three, including items like post-discharge medication review, advanced care planning, and functional status assessment rates.
What I would like to see are measures that cover Donabedian's structure, process, and outcome components of quality that could potentially give guidance on how to improve these plans after they get started. For structure, I think we should measure things like current levels of training in complex/geriatric care among providers, their real-time access to a shared care plan, and their ability to readily communicate among "team" members--including patients and families. For process, I would like to see measures of how long it takes providers to get critical information, such as when a patient is hospitalized and the results of ACOVE measures of geriatric syndromes. For outcomes, rates of ambulatory care-sensitive hospitalizations are good, but so is preservation of functional status and attainment of patient/family specified goals of care.
I know that these are not all National Quality Forum-approved measures that fall cheaply out of billing records. But we are proposing a multibillion dollar experiment with the lives of the most frail older and disabled people in the country. We shouldn't stint on measuring the things that matter to them and to getting this quest for the Holy Grail right.
As always, I hope you will comment on this post, but much more I hope you will go to the web page for the office of the duals, read one of the state proposals, and click on the "submit comments" button to give your two cents. Together, we can find—or rather, create—the Holy Grail of coordinated care. Act soon; the public comments period has already closed for a third of the plans.
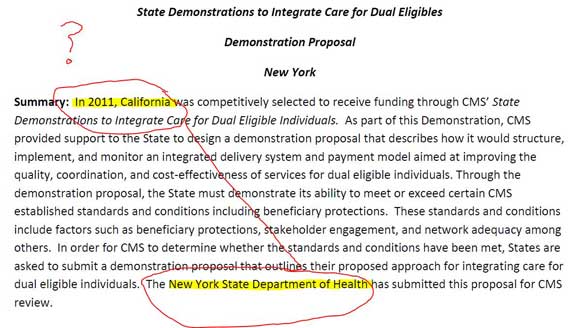
Oh, and P.S.--can anyone tell me why the New York plan starts out talking about California? A little cut and paste got out of hand perhaps?