Shortly after I was diagnosed with inflammatory breast cancer a scan showed a hot spot on my lower spine. Was it the spread of cancer? My oncologist scheduled a bone biopsy at my hospital, Maimonides Medical Center, in order for us to find out.
A few days before the procedure, I went in for preadmissions testing. As part of my formal intake, in addition to collecting my insurance information and poking and prodding me a few times, the nurse asked me if I would like to fill out an advance directive. This was not because she was a miraculous oracle who knew the outcome of my biopsy, which would leave me with a Stage IV diagnosis. No, her question was merely standard procedure. I said yes, and shortly, a specially trained social worker arrived to walk me through the process.
 The author and her mother, June 2011
The author and her mother, June 2011A cheerful young woman reminiscent of a camp counselor sat down next to me with papers neatly attached to her clipboard. The first step, she explained, is appointing a health care proxy, someone you trust to make health decisions for you should you become incapacitated. Being a nurse, I knew this, but it was comforting having someone there with me while I filled out the form. I chose my mother. Since my diagnosis, she and I had had numerous conversations about what I wanted should my disease progress and take away my quality of life. I trusted that she would respect my wishes, even if that meant making painful decisions as my disease progresses.
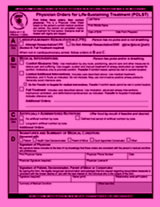 There is another form of advance directive that I haven’t completed yet—but will—with the assistance of that same social worker. It is nationally known as the POLST or Physician Orders for Life Sustaining Treatment. Developed in Oregon and disseminated by the California Healthcare Foundation, POLST turns the treatment wishes of seriously ill individuals into physician-signed medical orders that the health care team must follow.
There is another form of advance directive that I haven’t completed yet—but will—with the assistance of that same social worker. It is nationally known as the POLST or Physician Orders for Life Sustaining Treatment. Developed in Oregon and disseminated by the California Healthcare Foundation, POLST turns the treatment wishes of seriously ill individuals into physician-signed medical orders that the health care team must follow.
At the moment, I feel fine. I would want to be resuscitated, intubated, hydrated, and whatever else was necessary to get me back on my feet. Once the cancer begins to seriously compromise my health, however, I will fill out the POLST with instructions to limit my treatment to comfort care only.
Talking about our wishes when we are dying is hard. It’s hard for patients, families, and health care professionals. I look at the POLST form as a way of lightening the load on my family and on my health care team by informing them in advance of my treatment choices. It also offers the added bonus of ensuring that the treatment I get is the treatment I want, not what others think I want.
Even though filling out the POLST is reserved for those at the end of life, I believe everyone should know what is in it. It makes a great starting point for discussions with the friend or family member you intend to appoint as your health care proxy—which everyone, even the young and healthy, should do.
After discussing the POLST form with me, my mom said that she never knew you are allowed to refuse antibiotic treatment for pneumonia and other infections at end of life. While I am not suggesting that everyone would choose this, I would prefer to limit prolonged suffering. My mom would as well.
Once I filled out my health care proxy form, the social worker advised me that it would stay on file at the hospital and with my oncologist. She recommended that I give copies to my mother, my primary care physician, and anyone else or any other institution involved in my care. (And as a reminder, Mom, I keep a copy in my top dresser drawer.)
The social worker left me feeling empowered and positive. Later that week when I found that cancer had in fact spread to my spine, I was comforted to know that the care I will receive will be the care I choose. In my remaining lifetime I would like to see more hospitals, oncology centers, and nursing homes adopting Maimonides’ wonderfully integrated approach to advance directives. They didn’t wait until I had the terminal diagnosis or was hooked up to machines in intensive care, when health care decision-making is fraught with stress and fear, to ask. Instead, they made it part of their routine and trained a staff member to work with patients and explain the issues.
Why can’t this practice be more widespread? Why can’t all other patients in my position and all older adults have access to this vital yet simple service? Why do policymakers advocate for patient-centered care while letting “death panel” nonsense stifle the conversations that would help patients make informed treatment decisions? The expense is minimal—some forms and one terrific social worker—but the peace of mind it affords patients is priceless.
Fourth in a series. See also:
