At the recent Grantmakers in Health (GIH) funders forum on health reform, we were privileged to have Atul Gawande as our kick-off speaker. (On the video, Lauren LeRoy, the CEO of GIH, introduces him as a “Rock Star” for the health policy set.)
As the brilliant staff writer for The New Yorker, Dr. Gawande often sets the terms of national health care conversation with pieces like Letting Go, on care at the end of life, and The Cost Conundrum, on regional variation in health care spending. A bit less prominent but very near to my heart were his 2007 piece on geriatrics, The Way We Age Now, and his 2009 piece on spreading innovation in health care, Testing, Testing. So I was very gratified that his talk was about the links between the two: how do we diffuse the innovations we already have—like models of high-quality care for older adults—across the health care system?
In Gawande’s analysis, we were all fundamentally deceived by penicillin. Because penicillin was an innovation that was difficult to discover but relatively easy to deliver, we developed unrealistic expectations about change. We thought that all you had to do was have a eureka moment in the biotechnology lab, then the innovation would deliver itself, rather than requiring profound organizational change or system redesign. (We are still learning this lesson as we try to implement health IT.) In this techno-centric concept, neither the public nor even leaders in the health care system perceive advances in system design and operations--such as the models of care funded for testing or dissemination by the Foundation--as the innovations they are.
Unfortunately for the spread of quality care, many of the chronic health issues that are most prevalent and most severe are the reverse of penicillin. These are cases where we already have a relatively technically simple solution, but we lack the systems to deliver it reliably on a national scale. For example, providing complete guideline-concordant care to everyone with asthma, coronary artery disease, or chronic obstructive pulmonary disease (COPD) would improve outcomes well beyond the likely benefits of the next incremental improvement in medications. Or, take depression: the Foundation's IMPACT model doubles the effectiveness of the widely prescribed anti-depressant medications used in usual practice models. Yet as a nation we only meet standards of care perhaps 60% of the time. In many cases, it is actually against the economic interests of health care organizations to do better. In his own work, this emphasis on systems engineering is behind Dr. Gawande’s Checklist Manifesto--simple organizational techniques that ensure that our powerful biotechnology is delivered at the right time and right place, every time.
We seem to have an expectation that technology will magically fix health care, but the reality is that the potential value of biotechnological innovation is not realized if it’s applied within a dysfunctional system. Our health care systems remain at the artisanal level--fragmented, run by fiercely individualist craftspeople, riven by guild protections about who can do what, and extraordinarily variable across the country. Think of the variation in labor force between NYC, where you can’t swing a cat without hitting a physician sub-sub-specialist, to Alaska, where specialists are few and far between.
So what do we do?
The way that Dr. Gawande poses the question is, “How will the 13,000 service lines of health care be delivered reliably to EVERYONE?”
He proposes this formula:
1. Set a clear, intentional goal of improvement.
2. Because of regional variation, address change locally. Regions must create platforms for stakeholders to come together.
3. Get local data to inform the local coalition. Although regional differences might not be that big, everyone will be more motivated if they are working on what's important locally.
4. Find the existing systems innovations that address local concerns and goals.
5. Build a consensus to execute, to persistently make change, even in the face of reverses and opposition.
These efforts will help create a virtuous cycle of development that will forge a more functional health care system out of our current chaos, a system capable of making more and more powerful changes.
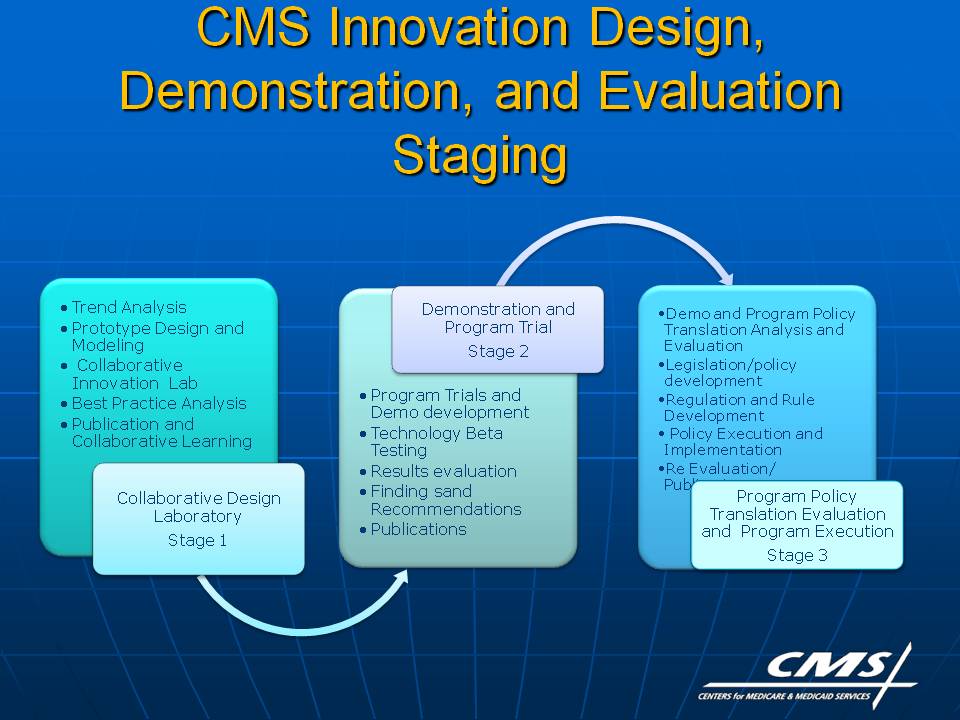
Given Dr. Gawande’s role in health care, I was not surprised when I realized that this vision of locally led, iterative change is the emerging vision (see this PowerPoint) of the new Center for Medicare and Medicaid Innovation under development at the Centers for Medicare and Medicaid Services this year.
If this is indeed the framework that emerges from the Center for Medicare and Medicaid Innovation, we will be very concerned to bring to its Collaborative Innovation Labs the ideas, leaders, and evidence we have helped foster over the years. If we can all work together, we can reduce avoidable suffering, increase the value of health care spending, and spring into the future. Boing!
