 Older Americans are not getting very good quality health care, as findings from many studies and experts show. However, most older adults and their caregivers don’t realize that they are getting substandard care. Given that most people are unfamiliar with the various guidelines for the treatment of chronic conditions and geriatric syndromes (e.g., falls, dementia, incontinence), it is probably unreasonable to think that they will ever be able to judge if their care is meeting evidence-based standards. People tend to mistake easy access to interventions (and particularly specialist physicians) for quality.
Older Americans are not getting very good quality health care, as findings from many studies and experts show. However, most older adults and their caregivers don’t realize that they are getting substandard care. Given that most people are unfamiliar with the various guidelines for the treatment of chronic conditions and geriatric syndromes (e.g., falls, dementia, incontinence), it is probably unreasonable to think that they will ever be able to judge if their care is meeting evidence-based standards. People tend to mistake easy access to interventions (and particularly specialist physicians) for quality.
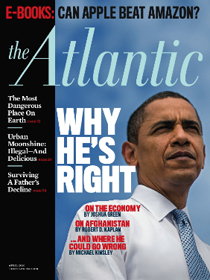 When family caregivers need to take on a substantial share of care for their loved ones, the many deficiencies in our system become very apparent to all concerned. This reality is poignantly captured in a first-person story in the April 2010 Atlantic Monthly, "Letting Go of My Father," by Jonathan Rauch.
When family caregivers need to take on a substantial share of care for their loved ones, the many deficiencies in our system become very apparent to all concerned. This reality is poignantly captured in a first-person story in the April 2010 Atlantic Monthly, "Letting Go of My Father," by Jonathan Rauch.
As Mr. Rauch struggles with caring for his father in his last year, he identifies many of the issues caregivers face. He writes, "My professional work all but stopped. Finding doctors for him and getting him to appointments and coordinating escalating medical needs swallowed entire days." As a caregiver he struggles with not only his father's care needs, and the weaknesses of the care system, but his own lack of preparation for the caregiver role. He writes "The medical infrastructure for elder care is good, very good. But the cultural infrastructure is all but nonexistent. How can it be that so many people like me are so completely unprepared for what is, after all, one of life's near certainties?"
The juxtaposition of those two quotes reflects most Americans’ misperception of quality of care. How can the "medical infrastructure" be "very good" when it requires Mr. Rauch to spend entire days "coordinating escalating medical needs?" I think the paradox shows the low expectations and excessive credit we all typically give the "medical" system. In an objective analysis, a health care system that depends upon untrained family caregivers for "coordinating escalating medical needs" is neither safe nor effective.
At the Foundation we have been trying to improve this situation by increasing geriatric care competence of the health care workforce in many ways. As part of this broad effort we have specifically been trying to improve the preparation of health professionals to support family caregivers. First, we supported a “state of the science” process culminating in a special issue of the American Journal of Nursing and the Journal of Social Work Education. Second, to implement the results, we supported the AARP Foundation in partnership with the Family Caregiver Alliance and the Administration on Aging.
But I certainly agree with Mr. Rauch’s point about the cultural infrastructure. As he ruminates upon how our society could do better, Mr. Rauch compares the cultural change we need around elder care to that demanded by feminists in the 1960s to overcome the loneliness and isolation of the role of housewife. He suggests that the first step is to build awareness of the common problem, taking it from the domain of the purely personal to the societal level so that we can find systemic solutions, much as Betty Friedan did in her book, The Feminine Mystique. He calls for a wide range of social changes, such as caregiver-friendly corporate policies, greater willingness to ask for and accept help, and proactive efforts to prepare people for a likely role in elder care.
But most of all, he calls for increasing public awareness: "What we need … is for our nameless problem to be plucked out of the realm of the personal and brought into full public view, where help can find us. . . By keeping the problem out of sight and consigning it to the realm of the 'personal,' the culture enables our natural tendencies to denial, procrastination, and silence."
 Today we celebrate the first step on this path of culture change with the launch of the Atlantic Philanthropies’ Campaign for Better Care.
Today we celebrate the first step on this path of culture change with the launch of the Atlantic Philanthropies’ Campaign for Better Care.
"The Campaign for Better Care has already built a broad-based consumer coalition of more than 100 powerful organizations and is supported by a wide range of stakeholder allies. Led by the National Partnership for Women & Families, Community Catalyst and the National Health Law Program, with funding from The Atlantic Philanthropies, we will work with policymakers to implement reform in ways that ensure that the people who are the sickest and most vulnerable – and their family caregivers – get the comprehensive, coordinated health care they need and deserve."
Recognizing the need for a social movement that will take on these issues at all levels, from grassroots opinion to legislative policy, the campaign adds public engagement to the set of strategies that the elder care community is employing to improve the lives of older Americans. We at Hartford have long wished for such an effort that would "open a new front" in the struggle and coordinate with our health professions and workforce strategies. I deeply hope that the work of our grantees and the Foundation can achieve synergy with the Campaign and that together we will make great strides.
