While reading the article "Desire in the Twilight of Life" in the Wall Street Journal, by Mark Lachs, MD, director of geriatrics for the New York-Presbyterian Healthcare System and professor of clinical medicine at the Weill Cornell Medical College, I was reminded of a lively dinner conversation with a group of friends, most of whom also work in the field of aging. My friend, a geriatric psychologist, commented that all medical and psychological exams of older people should include an inquiry about sexual activity. Our friend, a geriatrician, vehemently disagreed, stating that most of her patients are so frail, and many demented, that it would not be necessary to ask. They argued back and forth for a bit, when I interjected a relevant story about my grandfather.
My grandfather‘s second wife (he was widowed), Gladys, was in the last stages of Alzheimer’s disease when we shared a two-family house in New Jersey. I saw Gladys every day. She and I had a special love for each other, and when I came home after work her whole face lit up in recognition. She couldn’t speak, but we would sit and hold hands while watching TV. One night my grandfather came into the room, and I felt and saw Gladys cower and become frightened. Knowing my grandfather, I surmised the reason. I took him aside and told him he had to stop having sex with Gladys. He became angry and said that it was his wife’s duty. I explained that she couldn’t willingly consent to have sex with him and that in her confused state she probably didn’t know what he was doing and he might be hurting her. We talked about Gladys’s dementia and my grandfather’s needs. I convinced him to see a counselor. Fortunately I knew a wonderful geriatric social worker who worked with families of Alzheimer’s patients. My grandfather met with her many times and I could see him change in his behavior towards Gladys.
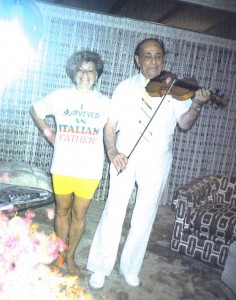
Both the counselor and I gave my grandfather permission to date and to seek sexual relations with someone other than his wife. My grandfather and Gladys moved to Florida, and I soon began getting calls from him telling me about his dates. He was having fun dating a good friend of his and Gladys’s, and she stood beside my grandfather when Gladys was buried.
Unfortunately, my grandfather broke up with this lady friend when he met a much younger woman, Estrella. Soon my 90-year-old grandfather was engaged to a 55-year-old woman. He bought Estrella a condo, a Cadillac, fur coats, and jewelry. I was worried, but he wouldn’t listen. He changed his will and made Estrella his sole heir.
One day, however, my grandfather called my mother and said he’d had a bad premonition. He was heading to his lawyer’s office to change back his will, cutting off Estrella. The next day he was found unconscious on the floor of his bathroom, and he died shortly after. Estrella managed to forge and cash two checks; then she and her husband (from whom she was supposed to have been divorced) fled with her car, furs, and jewelry. It could have been much worse. At least my grandfather did rewrite his will, leaving everything else to his four daughters and nothing to Estrella.
This very tragic yet all-too-typical story highlights two key areas of Mark Lachs’s research: sexuality and older people and elder abuse. Gladys was a victim of a form of elder abuse until my grandfather accepted guidance from a knowledgeable social worker. Then, my grandfather was a victim of financial abuse. Both of these incidents were the result of the sexual needs of an older man. A recent article in the Annals of Internal Medicine, discussed on the GeriPal blog, showed that sexual activity in older adults is more prevalent than most people think. Therefore, I believe it is very important for doctors to discuss sexual activity with older people and/or their family/caregivers, not only because it is an important component in a relationship, but also because it could uncover hidden family dilemmas that need to be brought to light.
In addition to the need for health care professionals to have basic information on older adults and sexuality, it is also important to have knowledge of elder abuse. The Elder Justice Act (EJA) was enacted as part of the Patient Protection and Affordable Care Act (PPACA). It sets forth a series of provisions designed to address some of the weaknesses in federal and state efforts to prevent and respond to abuse, neglect, and exploitation of older people. The National Health Policy Forum provides an excellent summary of the Act here.
I can’t stress enough the need to have discussions about sexual needs and activity and possible abusive situations with all older people. The more that all people are informed, the more we can prevent incidents like the ones that Gladys and my grandfather had to endure.
