Last week I attended the first annual meeting of the Long-Term Quality Alliance and listened to Gregg Pawlson (a geriatrician and executive with NCQA) talk about quality measurement. Right now, quality measurement does too little to drive practice towards quality care because it is based only on things that are “feasible,” or easy to measure—like what gets coded on medical bills. Pawlson observed that while feasibility must be one of the watchwords of quality measurement for now, in the near future electronic medical records should allow us to move beyond billing codes to gather real clinical data for more important quality measurement, including key care processes and outcomes.
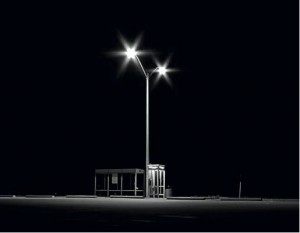 I sure hope so. Because those who have looked beyond the dim illumination of current billing-based “quality measures” and searched in the darkness where real processes of clinical care can found have found that the situation is grave. The ACOVE (Assessing Care of Vulnerable Elders) process, while laborious, looks at clinical care where it really happens - in offices and charts - rather than in bills and therefore has a better chance of driving meaningful quality improvement. Readers of Health AGEnda know that I am a big fan of this work, begun at RAND by outstanding clinician-researchers including Neil Wenger, David Solomon, David Reuben, and many others. I believe that ACOVE is an example of what we need in elder care: high quality evidence about essential clinical practices that are sensibly related to real health outcomes and show how we could (often easily) do better for older people. ACOVE is a blessing.
I sure hope so. Because those who have looked beyond the dim illumination of current billing-based “quality measures” and searched in the darkness where real processes of clinical care can found have found that the situation is grave. The ACOVE (Assessing Care of Vulnerable Elders) process, while laborious, looks at clinical care where it really happens - in offices and charts - rather than in bills and therefore has a better chance of driving meaningful quality improvement. Readers of Health AGEnda know that I am a big fan of this work, begun at RAND by outstanding clinician-researchers including Neil Wenger, David Solomon, David Reuben, and many others. I believe that ACOVE is an example of what we need in elder care: high quality evidence about essential clinical practices that are sensibly related to real health outcomes and show how we could (often easily) do better for older people. ACOVE is a blessing.
One of the leaders of the ACOVE program is Neil Wenger, MD, a faculty member in General Internal Medicine at UCLA and a researcher at RAND whom I have cited in my posts. However, in his talk to the Maxwell School of Public Policy at Syracuse University (another treasure I found last fall at GSA), he really outdid himself in delivering one of the most accessible (and provocative) descriptions of this research program I have ever read. He asks, "Do We Want to Measure the Quality of Care for Vulnerable Older People?" Given the lack of attention to the ACOVE work, I understand his frustration.
Neil and the ACOVE researchers wanted to focus specifically on the care of vulnerable elders, that 10-20% of older adults for whom the quality of care makes the most difference. For these persons, the ACOVE team asked itself what health care processes were a) supported by reasonable evidence, b) not contraindicated by common issues in an aging population, and c) likely to make a difference in the health outcomes of older people. For example: IF a vulnerable elder has had two or more falls in a year or one fall producing an injury, the causes of the fall should be assessed, BECAUSE falls are strong predictors of decline and death and many of their causes are modifiable. So if an older adult meets this criterion, his or her health care team should perform a get-up-and-go test for gait and balance problems, assess orthostatic hypotension (by taking blood pressure measurements lying down and then upon standing), etc. Dr. Wenger argues that the main thrust of the ACOVE process is very conservative in that its objective is to identify processes of care that if not provided to a patient meeting criteria almost always indicate a problem in quality of care.
The amount of work that has gone into ACOVE is truly astounding. Field researchers have reviewed thousands of patient charts looking for the hundreds of trigger conditions (e.g., two or more falls in 12 months) and then looking for the presence or absence of indicated processes of care in the records. These reviews have been performed in multiple health systems around the country, as well as by other research teams, and the findings seem remarkably consistent. For the general medical conditions like diabetes or hypertension, the quality of care is as Elizabeth McGlynn found it in her classic New England Journal article – around 55% of indicated care is provided. However, for the geriatric syndromes – things that are not caused by a single disease, but rather by common systems failures in aging humans, e.g., falls, incontinence, or cognitive impairment – the average proportion of indicated care provided is only 30%.
Completing the picture, the ACOVE team has shown that differences in quality of care are related to life or death--i.e., vulnerable older people getting higher quality care live longer than those who don’t--and that practice improvement interventions (e.g., ACOVE PRIME) can improve the likelihood of a medical practice delivering this kind of care. Not only did Dr. Wenger summarize this work in his Maxwell talk, but David Reuben used it as the basis of his Freeman award lecture at GSA in 2009. Vineet Arora has used the framework to look at processes of care for hospitalized elders, and Cliff Ko is using his training in the method to develop quality indicators for surgery in older adults as the head of quality improvement at the American College of Surgeons. The ACOVE framework has generated an impressive body of descriptive, intervention, and measurement tools.
So why does nobody know about this work? Because it is defined as “unfeasible.” Because ACOVE looks for our keys to quality in the dark—where we know they are—rather than under a streetlight just because it’s easier to look there. And because the assessment of quality is based on the process of chart review (and having read and extracted nursing home charts, I know how laborious this can be), the ACOVE process is just dismissed as impractical when compared to the less useful and less important computerized processing of things that turn up in billing records – did a diabetic get an eye exam or have a cholesterol test. It's not that I (or the ACOVE group) think those standard measures are useless; they are just not as useful. Among other things, they don't provide directions for useful change in practice. Moreover, I think it is fair to say that judgments of feasibility are dependent upon will and infrastructure. As long as quality of care for vulnerable elders is not a priority, we will not have the information systems that will make it easy to look at important processes of care. As a society, we have made choices as to how health care is monitored and what systems we have for quality measurement. We have decided where the streetlights should go to make it easy to search and what they will leave in the dark. I think we should choose again.
