“Everything old is new again” can be said with a sneer and imply that the same failed proposal is being offered once again--as in, “Accountable Care Organizations are just 90s-era managed care warmed over.” Or it can be said with joy and a wonder that the value of prior work endures and that we may have yet another chance to get it right.
 Close readers of HealthAGEnda might recall my comment on the potential value of the National Chronic Care Consortium’s work to this next generation of integrated health systems. And to my great pleasure a couple of weeks ago, I saw the equivalent of a phoenix rising from the ashes of the National Chronic Care Consortium (NCCC), suggesting that the ideals of the NCCC have been reborn. On CMS’s Partnership for Patients website, at the bottom of its page of web links among the tools for improving care transitions, was a link to the NCCC.
Close readers of HealthAGEnda might recall my comment on the potential value of the National Chronic Care Consortium’s work to this next generation of integrated health systems. And to my great pleasure a couple of weeks ago, I saw the equivalent of a phoenix rising from the ashes of the National Chronic Care Consortium (NCCC), suggesting that the ideals of the NCCC have been reborn. On CMS’s Partnership for Patients website, at the bottom of its page of web links among the tools for improving care transitions, was a link to the NCCC.
The NCCC was a group of leading-edge health systems from the early 1990s who foresaw the need to shift from acute disease to chronic care and to integrate care across the full continuum, from primary to acute to home care and long-term care. They came together to share what they learned and help each other pursue the sometimes very counter-cultural path they had chosen. Organizations and leaders like June Simmons, then of Huntington Hospital (now at Partners in Care Foundation), Nancy Whitelaw of Henry Ford Health System (now of the National Council on Aging), Chris Fordyce (Himes) of Group Health Cooperative of Puget Sound, and Cheryl Phillips, then of Sutter Health System (now of LeadingAGE [until recently AAHSA]), created a vision of better care for people at higher value to society.
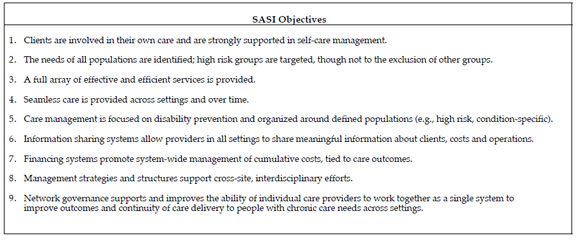
The Robert Wood Johnson and John A. Hartford Foundations were NCCC’s major external funders. RWJF was working under its large chronic disease initiatives and JAHF under its aging and health program, but with careful attention to what we were learning in our health care cost and quality program. JAHF made grants in 1991, 1993, and 1996 for a total of $1,000,000 (back when that was real money). The final grant supported the development of a tool intended to help organizations live up to their commitments to integration: the SASI Tool (Self Assessment for System Integration). Its nine objectives, seen in the box below, seem as fresh as ever in a world of electronic health records, care transitions, accountable care organizations, and medical homes.
But by the late 1990s, despite their importance, these ideas fell out of favor as the Clinton health reform package failed and the managed care backlash threw out the care coordination baby with the gatekeeping bathwater. The tide of system integration with its goals of better care coordination and higher value ebbed in favor of local maximization of benefits to parts of the delivery system and little attention to the whole and the overall patient experience. By 2003, with major member organizations no longer able to afford either the cash costs of membership or see the relevance of the vision to their day-to-day challenges, the NCCC board voted itself out of existence.
But neither the NCCC leaders, their ideas, or even the NCCC website and products ever went away--they have been with us all along, helping to drive the health system towards being a real system that can meet the ever more urgent needs of chronically ill Americans. Despite the collapse of the organization and the failure of our hopes for it, I’ve always been proud of the foundation’s relationship to the NCCC. I’ve even kept some NCCC souvenirs. If you ever see me in a hotel gym engaged in personal health promotion, take a close look at the blue band I use to hold my glasses in place.
I think that the SASI tool should become part of the the criteria for certifying Medicare Accountable Care Organizations. Can you think of a more clearly stated foundation defining the key components needed to integrate systems to provide better care for people with chronic conditions? I can’t, but please share if you can.