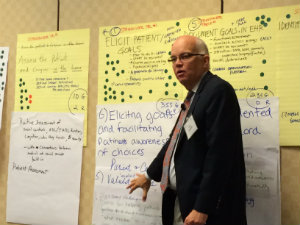
 Gary Oftedahl, MD, Chief Knowledge Officer for the Institute for Clinical Systems Improvement, speaks at the CaRe Align initiative launch in Dallas.
Gary Oftedahl, MD, Chief Knowledge Officer for the Institute for Clinical Systems Improvement, speaks at the CaRe Align initiative launch in Dallas.Older adults who typically live with many chronic conditions see, on average, two primary care providers and five specialists per year in four different medical practices. Such fragmentation and logistical complexities are problematic for providers and patients.
For a hypothetical primary care practice consisting of 30 percent Medicare patients, each of whom has four or more chronic conditions, the physician must coordinate with 86 other providers in 36 practices over a year’s time.
That’s a lot of cooks in the kitchen.
Different referral processes and incompatible electronic health record systems present a burden for both patients and providers that cause important communication gaps, duplication of testing, treatments, and confusion about clinical decision-making and accountability. Without clarity regarding communication and coordination responsibilities among health care professionals, patients and families/caregivers often have insufficient information to decide if treatment is consistent with their care preferences.
For medically complex older adults, treatments and medications are superimposed on people already being treated for a host of other conditions. Care given by each individual health care provider may be at cross purposes. One treatment can undo the good of another, or worse, cause injury. According to safety experts, older adults are the most vulnerable to needless harm or death when treatments conflict.
Whose goals and values should serve as true north for care and treatment decisions?
Increasingly, health care delivery is recognizing that the arbiter of true north is the patient. Person-defined goals are a way to align primary and specialty care to focus on what matters most to the people we serve. Patients are far more activated and engaged in their care when it focuses on achieving what matters most to them.
Whose goals and values should serve as true north for care and treatment decisions?
This may be less about particular clinical outcomes (e.g., lowering one’s blood sugar level) and more about living life the way they want (e.g., being able to garden). And the evidence bears out that activated patients have better health outcomes and lower health care costs.
Despite the challenges of primary-specialty-person-centered care coordination, this intersection represents a significant opportunity for improvement in the care of complex elders. To address these challenges and improve the value of health care for older adults, the John A. Hartford Foundation and the Patient-Centered Outcomes Research Institute (PCORI) have launched the CaRe Align initiative.
 About 50 health care leaders from around the country gathered for the CaRe Align launch.
About 50 health care leaders from around the country gathered for the CaRe Align launch.The 18-month planning grant aims to develop a feasible, sustainable, model that re-aligns primary and specialty care to meet the patient-defined goals of older adults with complex chronic conditions. The Hartford Foundation plans to test this new approach to care in the next phase of this initiative.
Key stakeholders—including providers, payers, patients, and families—are involved in the redesign. The team will:
- articulate a set of modifiable problems that influence quality, health outcomes, and health care costs for complex older adults; and
- determine the approach and corresponding evaluation plan aimed at improving care of complex elders through primary care/specialty care redesign.
The effort is co-led by Mary Tinetti, MD, director of the Hartford Center of Excellence in Geriatric Medicine at Yale University and co-led by Caroline Blaum, MD, chief of geriatrics at New York University School of Medicine.
Can Health Care Point to True North? At the recent launch of the CaRe Align initiative in Dallas, more than 50 leaders from around the country resoundingly answered, “Yes!”
