PRACTICE: Elizabeth
Twenty-seven years ago, the son of my housekeeper killed my daughter. She was fifteen. Everything changed in my life—completely. Before that I had happiness, a good family, everything was nice—but it turned into nothing. I was in shock.
For years and years I accumulated all the pain for myself. I tried to be strong for my son and my other daughter. My husband died six months later of a heart attack. So I found work to support my family. I thought I was strong and people told me I was strong. But it’s not true. I suffered. I cried. I was bleeding inside. I don’t know if people understand about depression. It puts your soul far away from you.
The years passed and I stayed in the same home. My children grew up and moved away. A year ago I lost my property. Before that I thought I could control everything. After that everything came on top of me and destroyed me. I tried to sleep and I could not. I felt like I was in a big bucket of oil trying to get out. I tried but I couldn’t. Life was terrible. I didn’t want to live anymore.
I went to Kaiser and said to my doctor, I’m depressed. She gave me pills, but they didn’t help. Then my doctor sent me to see Rita.
–Elizabeth
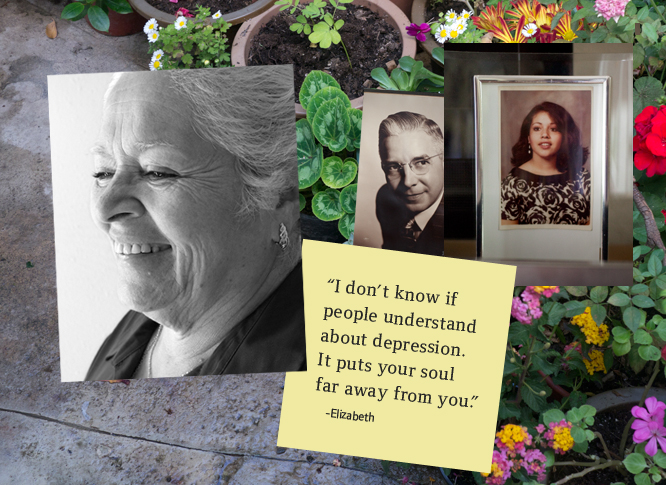
As part of the behavioral activation component of the program, she made a plan to contact her sister with whom she had not been in contact for many years. Elizabeth showed incredible improvement. We use a depression rating scale called the Patient Health Questionnaire to assess and track patient’s progress over time. Elizabeth’s score was originally very high at 24 and it went down to 1. She’s continuing to do well.
Rita Haverkamp, RN, MSN, CNS
Depression Care Manager
Kaiser Permanente, Southern California
A Clinical Practice Model that Changes Lives

Elizabeth
Primary care practices offering IMPACT also have a consulting psychiatrist assigned to the practice. The psychiatrist advises the depression care manager and primary care physician on treatment plans and meets directly with patients, if needed.
 Primary care physicians may have just a few minutes to explain depression and its treatment to a patient. Depression care managers can offer much more time. They can discuss how the depression is affecting the patient’s life and recommend strategies. This made a big difference for Elizabeth, who attributes her recovery from depression to her depression care manager, Rita Haverkamp. In addition to individual counseling sessions, Ms. Haverkamp offers a depression class (a form of group therapy). Elizabeth attended the depression class and sat quietly at first, letting others talk. Gradually she began to tell her own story. After many years of trying to protect herself from the pain of her loss by isolating herself, Elizabeth began to trust others. “Rita helped me to open up and feel like a person again,” says Elizabeth. “She came into my life to save my life. She’s an angel to me.
Primary care physicians may have just a few minutes to explain depression and its treatment to a patient. Depression care managers can offer much more time. They can discuss how the depression is affecting the patient’s life and recommend strategies. This made a big difference for Elizabeth, who attributes her recovery from depression to her depression care manager, Rita Haverkamp. In addition to individual counseling sessions, Ms. Haverkamp offers a depression class (a form of group therapy). Elizabeth attended the depression class and sat quietly at first, letting others talk. Gradually she began to tell her own story. After many years of trying to protect herself from the pain of her loss by isolating herself, Elizabeth began to trust others. “Rita helped me to open up and feel like a person again,” says Elizabeth. “She came into my life to save my life. She’s an angel to me.
Elizabeth carries the book When Bad Things Happen to Good People, which Ms. Haverkamp recommended, wherever she goes. Regularly reading passages helps her to cope. “From reading the book I realized it’s not only me. The book helped me to open my heart.
What is Depression?
Most people who suffer with depression experience prolonged, strong, pervasive feelings of sadness. Not just having a bad day, but a state that they can’t find their way out of. They may also lose interest in things that are important to them, like their children and grandchildren. Nothing that used to give them pleasure makes them happy. Some people with depression have other feelings, like feeling guilty, like they’re in other people’s way, like the world would be a better place without them. They may feel worthless and helpless. People who are depressed often don’t eat well because of a lack of appetite. They may lose weight. They often don’t sleep well. They feel like they have no energy, and they have difficulty concentrating. Being in a state like that for weeks on end can become overwhelming. (Major depression is diagnosed when symptoms persist for two weeks or more.) Some people start having thoughts of death and suicide. Most of the 36,000 people who commit suicide each year in the United States struggle with depression. Older men are the number one risk group for committing suicide.Older men may be less comfortable with identifying depression as a problem to a health care provider, and they are less likely to receive treatment for depression than women. In men, depression may also manifest slightly differently with higher rates of irritability and anger and higher rates of alcohol or other substance use.
Jürgen Unützer, MD, MPH
Director, Project IMPACT
Depression care managers are taught counseling strategies, called behavioral activation and problem-solving therapy. These counseling methods can be accomplished in a few short sessions and they can help a person improve with or without medication. Behavioral activation involves encouraging the patient to become active again, with exercise or things they enjoy. Ms. Haverkamp encouraged Elizabeth to set goals for ways she could improve her mood. During one of the depression classes, a participant mentioned that she wanted to contact her brother. “When I heard that it clicked in my mind, I have a sister in Oregon,” says Elizabeth. “I’d like to call my sister.” Elizabeth hadn’t spoken with her sister for 20 years. She was too depressed. “After she made that contact her sister invited Elizabeth to visit her in Oregon and she had a fabulous time,” says Ms. Haverkamp. The sisters are now back in touch and have a warm and supportive relationship.
Now my life is beautiful,” says Elizabeth. “I open my eyes in the morning and I don’t feel depression. I want to see my garden. I want to see how the flowers are growing. Life may not always be easy, but it’s good.”
Vernon’s Story
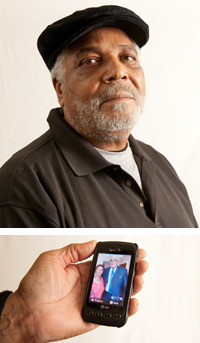
We had about six sessions, and we talked about some of the things holding me back. I had gotten to the point where I didn’t want to get up and do anything. He got me back out walking every day. It helped me a lot. I went on vacation to Virginia to attend my class reunion and spend some time with my daughter and two grandboys. I had a wonderful time. If I hadn’t gotten out of the mood I was in I wouldn’t have gone.
Since I came back I’ve started chemotherapy for prostate cancer. But it’s not affecting me like it affected me last year when I had it. I’m not depressed. I’m doing the best I can to fight it. My spirits are up. Without Jesse I don’t know what would have pulled me out of the depression.
Vernon, age 66
Client of Jesse Merjil, LCSW
Project IMPACT Depression Care Manager
LifeLong Over 60 Health Center
Oakland, California
Maria’a Story

As Maria’s depression care manager, I suggested some concrete tasks, such as going to a senior center in her neighborhood. Little by little she started making friends there. This gave her the self-confidence to address other problems in her life. Her sister who lived outside New York wanted her to move to the same state. Maria did not want to go. I used some problem-solving techniques with Maria, such as considering the pros and cons of such a move and thinking about why it was difficult for her to say no to her sister. We also did some role playing. I will never forget Maria’s relief after she told her sister she decided not to move. Maria has also become more assertive with her other sister.
Marcia Honigsztejn, LCSW
Project IMPACT Depression Care Manager
Woodhull Medical Center
Brooklyn, New York
A Proven Model
Elizabeth, Vernon, and Maria are by no means isolated cases. In fact, the IMPACT model was tested in a large study, the results of which were reported in 2002 in the Journal of the American Medical Association.1 About 1,800 older adults (average age, 72) with major depression, dysthymic disorder (a milder form of depression that lasts more than two years), or both who were being treated in primary care settings were enrolled in the study.
The study showed that the IMPACT team care approach more than doubles the effectiveness of the usual treatment for depression for older adults in primary care settings. Usual care involved treatment by a primary care physician or referral to a mental health specialist. After one year, about half of the participants in the IMPACT group reported a 50 percent or more reduction in depression symptoms, compared with 19 percent of those in the group receiving usual care. Patients improved at all 18 of the study sites.
Project IMPACT and this study were featured in the 2002 Hartford Foundation Annual Report (http://www.jhartfound.org).
Achieving Widespread Implementation

With an eight-year $2.4 million grant from the Hartford Foundation in 2004, the IMPACT Implementation Center was established at the University of Washington in Seattle to help health care organizations put the IMPACT model into practice. A set of tools was developed, including treatment manuals, job descriptions, and patient tracking and team building tools. The IMPACT Implementation Center also offers telephone consultations with staff and others who have already implemented IMPACT. The Center offers most materials free of charge on the IMPACT Web site (www.impact-uw.org).
The Center also developed a training program, which includes a two-day in-person workshop and a Web-based version of the program. There is a fee for these training activities, which has allowed the IMPACT Implementation Center to become self-sustaining. Over 5,000 clinicians have so far received this training. “This is an example of how foundation money can not only change something in health care but create something that sustains itself over the long run,” says Dr. Unützer.
The IMPACT model has been implemented in over 600 practices in more than 30 states, including Kaiser Permanente in Southern California, which serves three million members. Several large health plans have incorporated core components of IMPACT into their care delivery. One example of successful regional implementation is in the state of Minnesota with a state-wide initiative called DIAMOND (Depression Improvement Across Minnesota: a New Direction; www.icsi.org). Six Minnesota health plans agreed to finance this model of depression care, which has been implemented in more than 85 primary care clinics, reaching up to 1.5 million Minnesotans. IMPACT is now a benefit covered under these insurance plans in Minnesota.
The IMPACT model has been endorsed by national organizations, such as the Agency for Healthcare Research and Quality and the National Council for Community Behavioral Health.
Endnote
1. Unützer, J., Katon, W., Callahan, C. M., Williams, J. W. Jr., Hunkeler, E., Harpole, L., …Langston, C. (2002). Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. Journal of the American Medical Association, 288(22), 2836-2845.